Causes of Ear Infection Hearing Loss: An In-Depth Guide
Ear infection hearing loss is a common issue that affects millions of people worldwide. It can be a temporary or permanent condition, depending on the severity of the infection and how it is treated. In this comprehensive guide, we'll dive deep into the causes of ear infection hearing loss, its symptoms, and the best prevention and treatment options. With this information, you can make informed decisions about your health and ensure that you protect your hearing for years to come.
The Anatomy of the Ear: A Brief Overview
To better understand the causes of ear infection and hearing loss, it's essential to know the basic anatomy of the ear. The ear consists of three main parts: the outer ear, the middle ear, and the inner ear. Each section plays a crucial role in the process of hearing and maintaining balance.
- The outer ear includes the pinna (the visible part of the ear), the ear canal, and the eardrum.
- The middle ear contains three small bones called ossicles, which amplify sound waves and transmit them to the inner ear.
- The inner ear houses the cochlea, a spiral-shaped organ responsible for converting sound waves into electrical signals, and the vestibular system, which helps maintain balance.
Types of Ear Infections
Ear infections are typically classified into three categories, depending on the part of the ear affected:
- Otitis externa (outer ear infection): Also known as swimmer's ear, this infection affects the skin of the ear canal and is typically caused by bacteria or fungi.
- Otitis media (middle ear infection): This infection occurs when bacteria or viruses enter the middle ear, often as a result of an upper respiratory infection. It can cause fluid buildup and inflammation, leading to temporary hearing loss.
- Otitis interna (inner ear infection): Also called labyrinthitis, this infection is less common and usually results from a viral infection that spreads from the upper respiratory tract or bloodstream.
The Connection Between Ear Infections and Hearing Loss

Ear infections can cause hearing loss in various ways:
- Fluid buildup: Inflammation and fluid buildup from an ear infection can prevent sound waves from reaching the inner ear, resulting in temporary hearing loss.
- Eardrum damage: Severe or untreated infections may lead to a perforated eardrum, which can cause temporary or permanent hearing loss.
- Ossicle damage: Chronic middle ear infections can damage the small bones in the middle ear, impairing their ability to transmit sound and resulting in conductive hearing loss.
- Inner ear damage: In rare cases, an infection can spread to the inner ear, damaging the cochlea and causing sensorineural hearing loss.
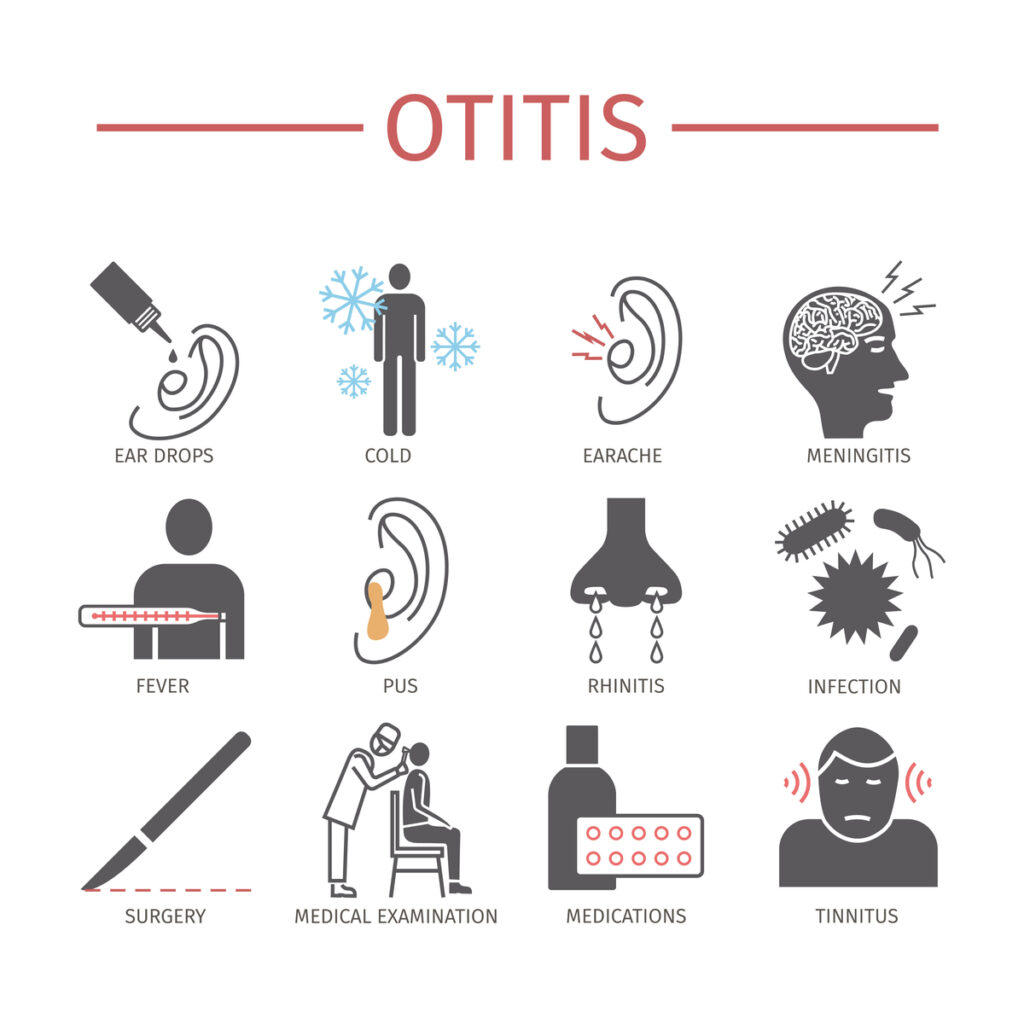
- Symptoms of Ear Infection Hearing Loss
The symptoms of ear infection hearing loss can vary depending on the type of infection and the severity of the condition. Common signs and symptoms include:
- Pain or discomfort in the ear
- Temporary hearing loss or muffled hearing
- Ear fullness or pressure
- Drainage of fluid from the ear
- Tinnitus (ringing in the ear)
- Dizziness or balance problems
- Fever
- Nausea or vomiting
Risk Factors and Causes of Ear Infection Hearing Loss
Several factors can increase the risk of developing ear infections and subsequent hearing loss:
- Age: Young children are more prone to ear infections due to their developing immune systems and smaller Eustachian tubes, which can become easily blocked.
- Upper respiratory infections: Colds and other respiratory infections can cause congestion and inflammation that lead to ear infections.
- Allergies: Allergic reactions can cause swelling and fluid buildup in the Eustachian tubes, increasing the risk of infection.
- Exposure to moisture: Frequent swimming or exposure to water can create a damp environment in the ear, encouraging bacterial or fungal growth.
- Smoking or secondhand smoke exposure: Tobacco smoke can irritate and damage the delicate tissues of the ear, increasing the risk of infection.
- Weakened immune system: Individuals with compromised immune systems are more susceptible to infections, including those of the ear.
Prevention and Treatment Options
To prevent ear infection hearing loss, consider the following strategies:
- Practice good ear hygiene: Keep your ears clean and dry, avoiding the use of cotton swabs, which can push debris further into the ear canal.
- Manage allergies: Seek treatment for allergies to reduce inflammation and fluid buildup in the ear.
- Avoid exposure to tobacco smoke: Quit smoking or minimize exposure to secondhand smoke.
- Vaccinate: Ensure children receive appropriate vaccinations to reduce the risk of respiratory infections that can lead to ear infections.
If you suspect an ear infection, consult your healthcare provider for a proper diagnosis and treatment plan. Depending on the type and severity of the infection, your doctor may recommend one or more of the following treatments:
- Pain relievers: Over-the-counter pain medications can help alleviate pain and reduce inflammation.
- Antibiotics: If the infection is bacterial, your doctor may prescribe antibiotics to kill the bacteria and prevent complications.
- Decongestants or antihistamines: These medications can help reduce congestion and inflammation in the Eustachian tubes.
- Ear drops: Prescription ear drops may be used to treat outer ear infections.
- Surgical intervention: In severe cases, surgery may be necessary to drain fluid from the middle ear, repair a perforated eardrum, or remove damaged ossicles.
When to Seek Medical Help
If you experience any of the following symptoms, seek medical attention immediately:
- Severe ear pain or sudden worsening of pain
- High fever
- Fluid or pus draining from the ear
- Sudden or rapidly worsening hearing loss
- Vertigo (spinning sensation) or difficulty maintaining balance
These symptoms may indicate a severe infection or complications that require prompt treatment to prevent permanent hearing loss or other health issues.
Final Thoughts
Ear infection hearing loss is a common but preventable condition. By understanding the causes and risk factors, you can take steps to protect your hearing and maintain overall ear health. If you suspect an ear infection, seek prompt medical attention to ensure the appropriate diagnosis and treatment, minimizing the risk of hearing loss and other complications.
Sources
- National Institute on Deafness and Other Communication Disorders. (2021). Ear infections in children. https://www.nidcd.nih.gov/health/ear-infections-children
- World Health Organization. (2021). Deafness and hearing loss. https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss